As an Amazon Associate ,I earn from qualifying purchase .
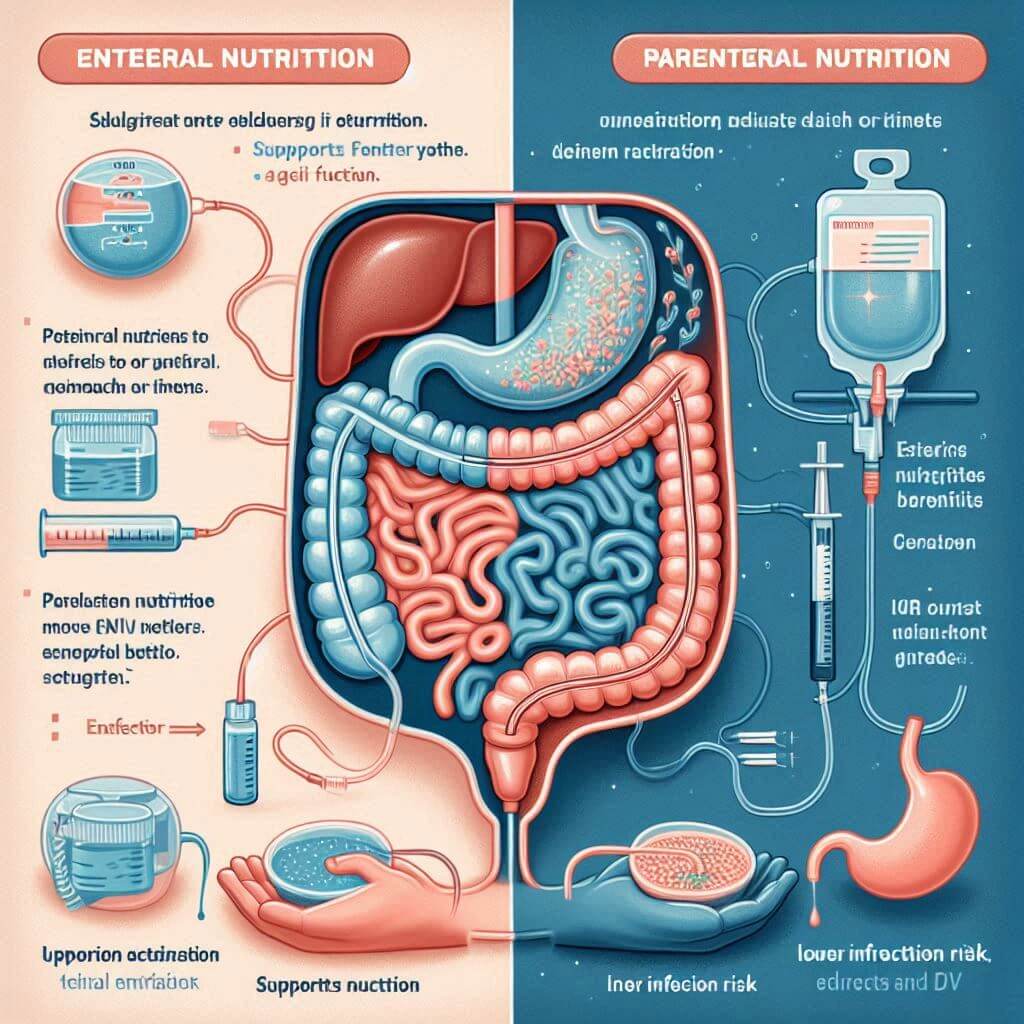
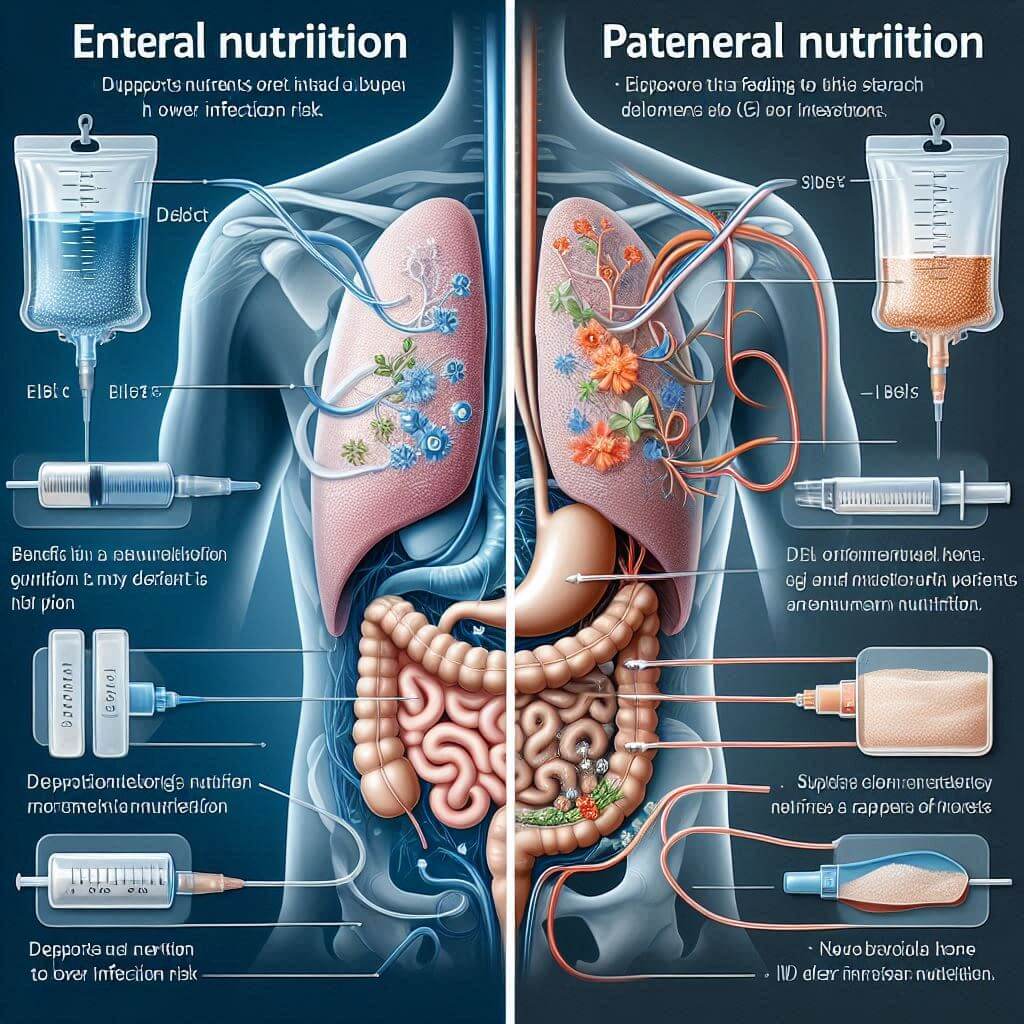
Nutrition plays a vital role in maintaining and restoring health, particularly for patients with specific medical needs. For those unable to consume food normally, Clinical Nutrition Options like Enteral and Parenteral Nutrition provide essential alternatives. Both methods support life and promote recovery, but each approach has unique attributes and risks. This article will provide an in-depth look at Enteral vs Parenteral Nutrition, covering their types, benefits, risks, and the considerations involved in choosing between them.

Understanding Clinical Nutrition: Why It Matters
Clinical nutrition encompasses dietary approaches aimed at improving health outcomes in patients with medical conditions that interfere with normal eating. The choice of nutritional support depends on individual patient needs, underlying medical issues, and specific nutrition requirements. Here, we discuss Types of Clinical Nutrition, specifically Enteral and Parenteral Nutrition, to help healthcare providers and caregivers make informed choices for optimal patient outcomes.
What is Enteral Nutrition?
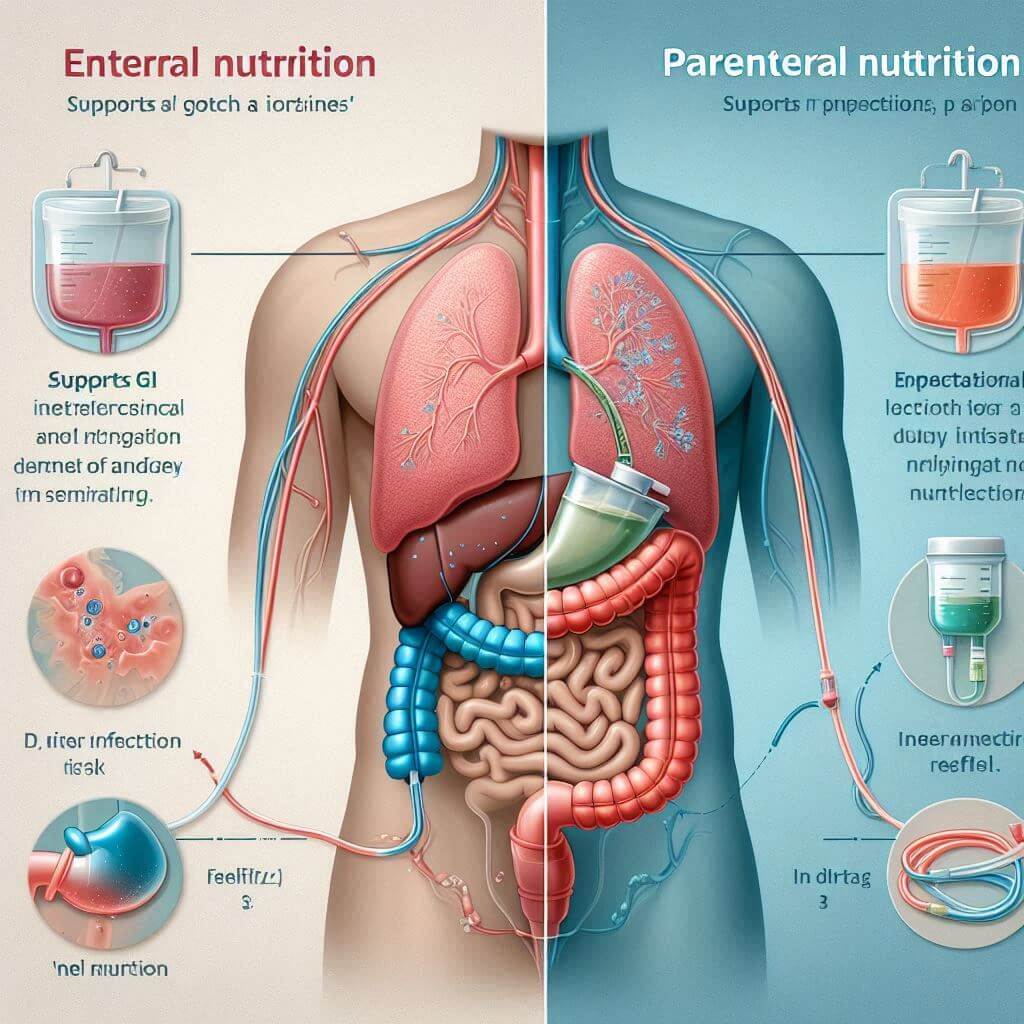
Enteral Nutrition, commonly known as tube feeding, delivers nutrients directly to the gastrointestinal (GI) tract via a feeding tube. This approach is recommended when patients cannot chew or swallow but still have a functional GI system capable of nutrient absorption.
Types of Enteral Nutrition
There are various forms of enteral nutrition based on tube placement and feeding methods:
- Nasogastric Feeding (NG Tube): A tube is inserted through the nose and extends to the stomach.
- Gastrostomy Feeding (G Tube): A surgically placed tube delivers food directly to the stomach.
- Jejunostomy Feeding (J Tube): In cases where the stomach cannot process food, a tube is placed in the jejunum.
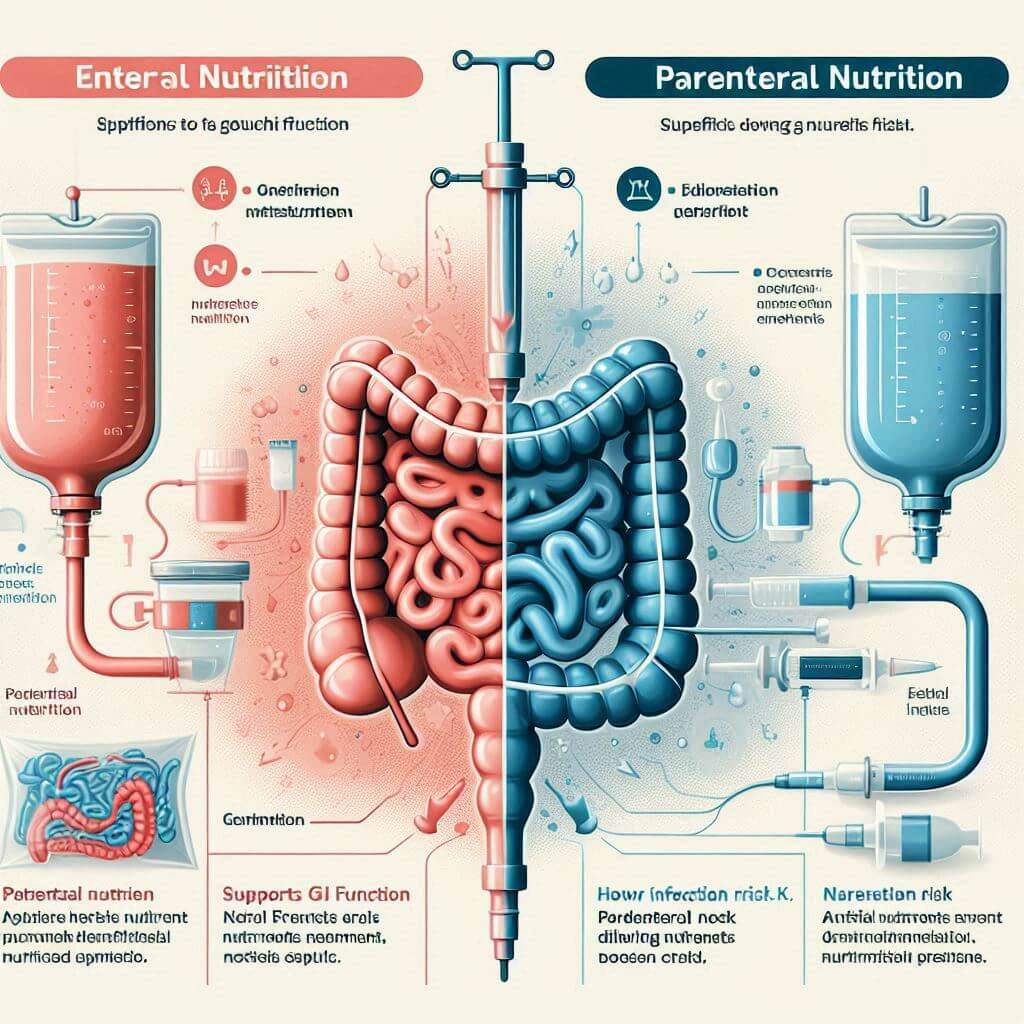
Enteral Nutrition Benefits
Enteral Nutrition Benefits are numerous and make it a preferred choice when feasible. Some key benefits include:
- Maintains GI Function: The GI tract continues to function and helps prevent issues like intestinal atrophy.
- Reduces Infection Risks: Enteral nutrition has a lower infection risk compared to intravenous methods.
- Supports Natural Digestion: Enteral nutrition mimics natural digestion by delivering nutrients through the digestive tract.
However, enteral feeding is only effective when the GI tract is functional and capable of nutrient absorption.
Pros and Cons of Enteral Nutrition
Like any medical approach, Enteral Nutrition has its advantages and disadvantages. Here’s a summary:
Pros:
- Preserves gut integrity
- Lowers infection risk
- Generally more cost-effective
- Provides nutrients in a manner similar to normal eating
Cons:
- Requires a functional GI tract
- Potential for aspiration pneumonia if feeding is not managed properly
- Discomfort or irritation at the tube site
What is Parenteral Nutrition?
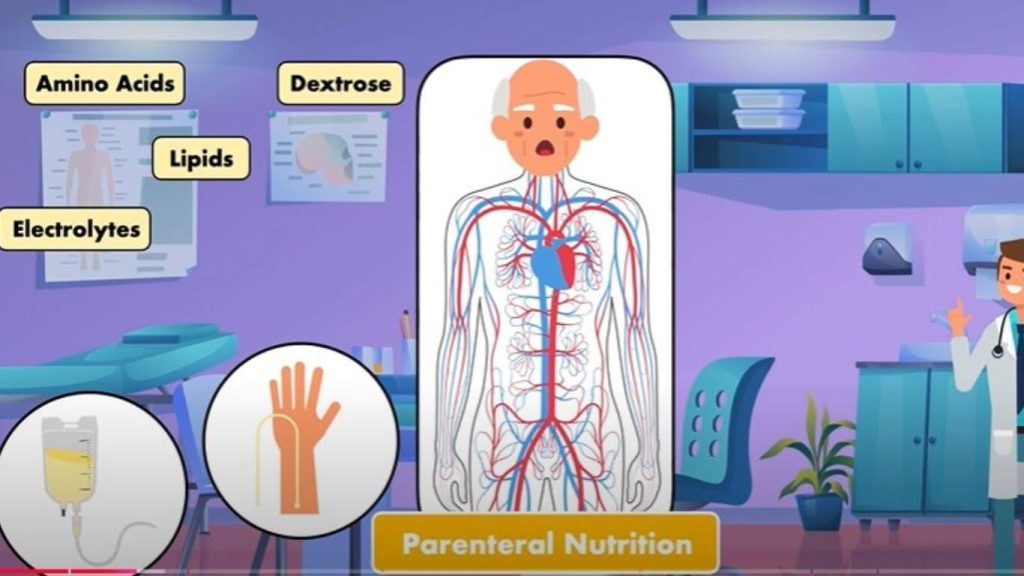
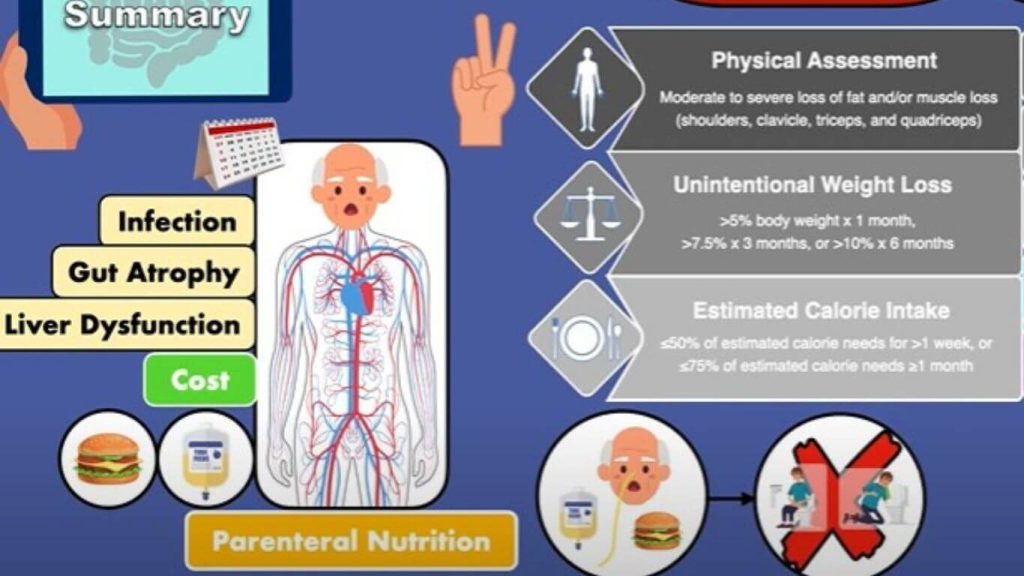
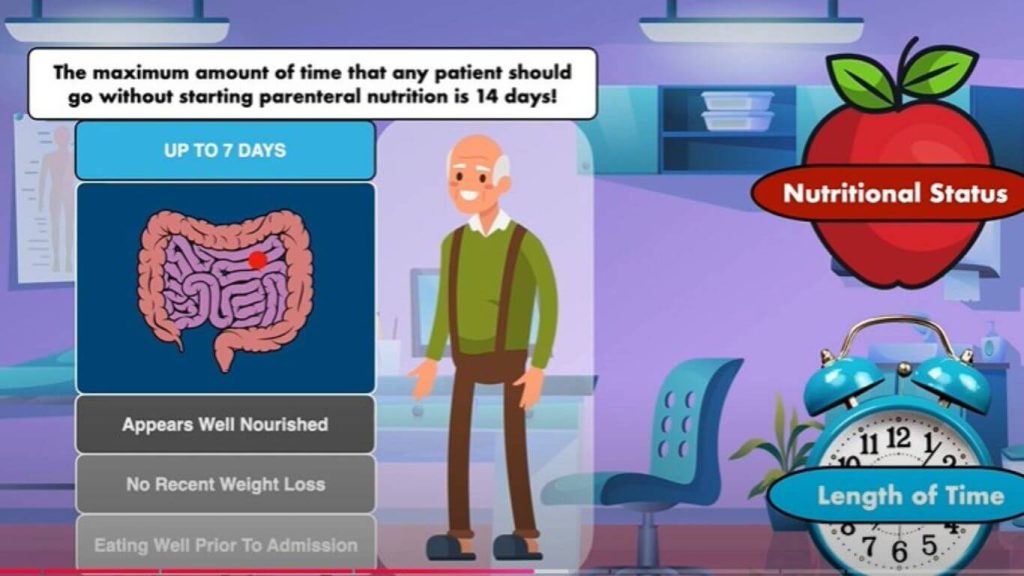
In contrast, Parenteral Nutrition (PN) involves administering nutrients directly into the bloodstream via an intravenous (IV) line, bypassing the GI tract altogether. This method is often used when a patient’s digestive system is nonfunctional or when enteral feeding is unsafe.
Types of Parenteral Nutrition
Parenteral nutrition options include:
- Total Parenteral Nutrition (TPN): Delivers complete nutrition intravenously, typically through a central line in a major vein.
- Peripheral Parenteral Nutrition (PPN): Supplies partial nutrition via a smaller vein, often used for short-term support.
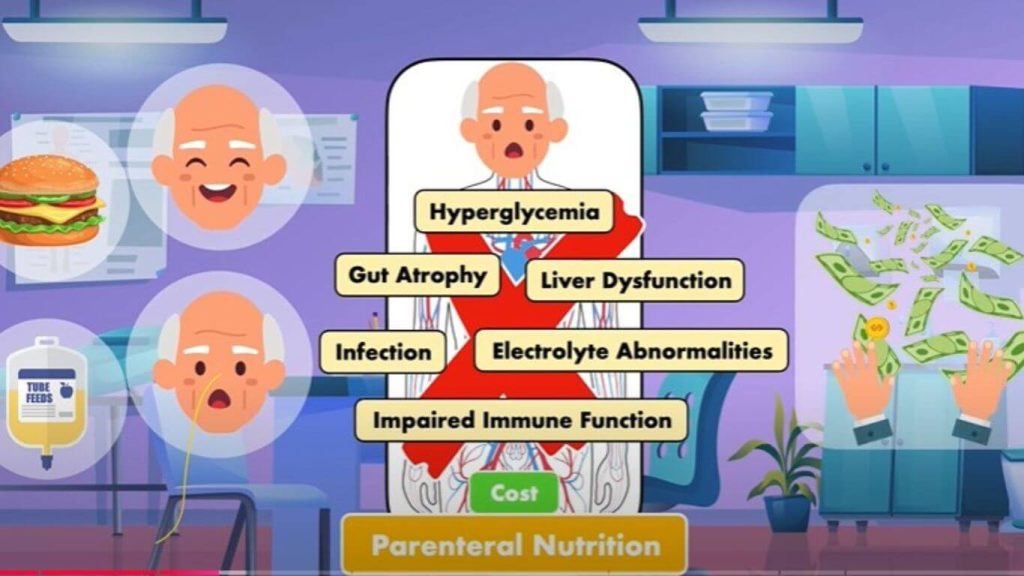
Parenteral Nutrition Risks
While life-saving, Parenteral Nutrition also carries specific risks:
- Infection Risk: Central lines, used in TPN, can introduce bacteria directly into the bloodstream, increasing infection risks.
- Liver Complications: Long-term parenteral nutrition can affect liver function, sometimes leading to liver disease.
- Metabolic Complications: Electrolyte imbalances, hypoglycemia, and hyperglycemia are common risks with TPN.
Due to these risks, parenteral nutrition is often considered when absolutely necessary and when the GI tract is nonfunctional or inaccessible.
Pros and Cons of Parenteral Nutrition
Evaluating the Pros and Cons of Parenteral Nutrition is essential for understanding its suitability in patient care:
Pros:
- Provides essential nutrients when GI tract use is impossible
- Can be life-saving in critical conditions
- Bypasses the GI system, suitable for patients with bowel obstruction or severe GI issues
Cons:
- High risk of infection, especially in central lines
- Expensive and complex administration
- Potential liver and metabolic complications with long-term use
Enteral vs Parenteral Nutrition: A Comparative Analysis
When comparing Enteral vs Parenteral Nutrition, several factors determine the best option for each patient. Enteral nutrition is preferred when the GI tract is functional, offering a safer, more cost-effective option with fewer long-term complications. Parenteral nutrition, on the other hand, is reserved for cases where enteral feeding is impossible.
| Aspect | Enteral Nutrition | Parenteral Nutrition |
| Delivery Method | Tube feeding into GI tract | IV feeding directly into veins |
| Infection Risk | Lower | Higher |
| Cost | Lower | Higher |
| GI Tract Integrity | Maintained | Not maintained |
| Complications | Aspiration risk, tube blockage | Liver damage, metabolic issues |
| Best for | Functional GI tract | Nonfunctional GI tract |
Nutritional Support for Patients: Choosing Enteral or Parenteral Nutrition
Selecting between enteral and parenteral nutrition is based on the patient’s medical condition, GI functionality, and overall health goals. Healthcare providers assess each case individually, considering the following factors:
- GI Functionality: If the GI tract works well, enteral nutrition is the first choice.
- Risk Factors: Parenteral nutrition is chosen in critical situations, but risks like infection and metabolic imbalances must be carefully managed.
- Patient Comfort and Long-Term Care: Enteral feeding is generally more comfortable and sustainable for long-term use compared to parenteral nutrition.
Tube Feeding vs IV Nutrition: Clinical Considerations
In the debate of Tube Feeding vs IV Nutrition, tube feeding is often preferred for patients who can digest and absorb nutrients but are unable to eat normally. IV nutrition is reserved for patients with severe gastrointestinal dysfunction where enteral feeding would not meet nutritional needs. While both methods aim to provide Nutritional Support for Patients, enteral feeding is typically less invasive and poses fewer risks.
Final Thoughts on Enteral vs Parenteral Nutrition
Choosing between Enteral vs Parenteral Nutrition is a critical decision in patient care. Each approach has distinct benefits and drawbacks, and healthcare providers must evaluate the patient’s unique needs, medical condition, and long-term health goals. Enteral nutrition is generally preferred when possible due to its lower risk profile and better support for GI health. Parenteral nutrition, while more complex and risk-prone, remains invaluable in specific cases where enteral feeding is not an option.
Ultimately, the goal of both enteral and parenteral nutrition is to ensure patients receive the nutrients they need to heal, recover, and thrive. With careful consideration and regular monitoring, these methods can be applied effectively to support diverse patient needs and improve quality of life in challenging medical circumstances.







2 thoughts on “Enteral vs Parenteral Nutrition: Guide to Improving Patient Health”